Effect of BRT with MEBT/MEBO on the Immunity of Burns Patien
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
The antibiotic and wound-healing properties of MEBO have been proven by clinical practice. There are different opinions about the mechanism of this antibiotic effect, so research on this subject is very important. During the period from January 1993 through December 1995, we conducted clinical observations on the effect of MEBO on burns patients’ immunity and demonstrated that MEBO enhanced patients’ immunity as part of its antibiotic and wound-healing effects.
MATERIALS AND METHODS
Clinical data:
One hundred and twenty burns patients were divided randomly into two groups. Sixty patients in the MEBO group, including 40 males and 20 females, aged 6 - 65 (35.5±14.8) years. Course of disease: 1 - 36 h (18.5±8.8h) before administration of MEBO. Cause of burn: direct flame, 30 cases; scald, 16 cases, and chemical burn, 14 cases. Burn position: craniofacial, 17 cases; neck, 17 cases; trunk: 18 cases and limbs, 23 cases. Burns depth: superficial second-degree burns, 26 cases; deep second-degree burns, 24 cases; third-degree burns, 10 cases. Burn area: 1 %~25 % (13±6 %) total body surface area (TBSA). By contrast, there were 60 cases in the control group including 41 males and 19 females, aged from 7 to 65 (36±14.5) years. Course of disease: 1 - 35 h (18±8.5 h) before administration. Cause of burns: direct flame, 29 cases; scald, 17 cases, and chemical burns, 14 cases. Burn position: craniofacial, 13 cases; neck, 7 cases; trunk, 18 cases, and limbs: 22 cases. Burn depth: superficial second-degree burns, 24 cases; deep second-degree burns, 26 cases, and third-degree burns, 10 cases. Burn area: 1~26 % (13.5±6.3 %) TBSA. The data of the two groups were similar and comparable (P>0.05).
Treatment and Examination:
All patients were subjected to debridement before collecting samples of skin tissue. Patients in the MEBO group were treated with burn regenrative therapy (MEBT/MEBO) [1, 2], and skin tissues were taken twice from the original sites before treatment began and after the wounds healed, respectively. Patients in the control group were treated with another traditional Chinese burns ointment--- Jing Wan Hong---, and skin tissue was taken at the same time phase as in the MEBO group. Patients in both groups were observed closely, and their wound healing time and incidence of wound infection were compared.
Five pieces of skin tissues taken from the edge of the burns wounds using a pair of biopsy forceps were immersed in 10 % formalin and kept in separate ice bottles, respectively. Four pieces of skin tissues were also taken from the normal (non-burned) skin of the same patient and treated identically as the other tissue. In addition, normal skin tissues from 60 surgical cases were taken during subdermal cyst operations and treated identically to both burns tissues. The levels of IgA-, IgG-, IgM-producing cells and C3 were determined using the frozen section immunohistochemical method. The first antibody was supplied from Vector and the second from DAKO. Venous blood samples of burns patients and healthy persons were taken in the morning before breakfast. Peripheral blood immunoglobulin (Ig) levels were determined using the agar diffusion method.
Classification Standard of Antibody Producing Cell and C3:
The classification standard was as follows: - = no positive cells or particles were found or only occasionally found in the whole slide; + = positive cells accounted for less than 30% of the total number of interstitial cells in the lamina propria; ++ = positive cells accounted for 31 ~70 % of the total number of interstitial cells in the lamina propria; +++ = positive cells accounted for more than 71 % of the total number of interstitial cells in the lamina propria. Histological diagnosis was based on the criteria stipulated at the China National Pathology Research Group Conference held in Zhengzhou in 1978.
RESULTS
1) Clinical Efficacy Assessment:
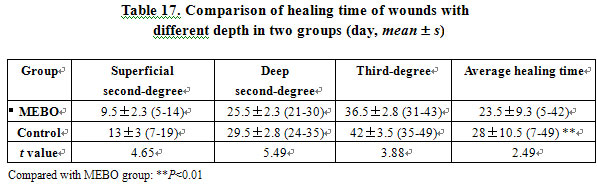
In the MEBO group, burns wounds with different depths had shorter healing time than those in the control group (P<0.01; Table 17). Only one case (1.7 %) in the MEBO group had wound infection, compared to 9 cases (15 %) in the control group. The difference between the two groups was significant (2=5.35, P<0.05). MEBO was proved to have infection-controlling and healing-promoting effects.
2) Experimental results:
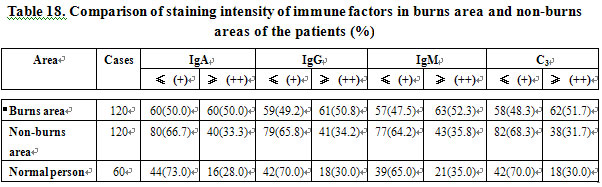
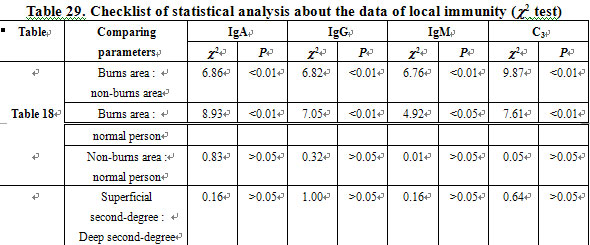
IgA-, IgG-, and IgM-producing cells and C3 in the burns area had higher staining intensity compared to those of the non-burns area and to those of normal persons (P<0.01). The immunity of the local area changed postburn. Immunologic function and reaction were enhanced. In the non-burns area, the immunity was similar to that of normal persons. The difference was not marked (P>0.05; Table 18).
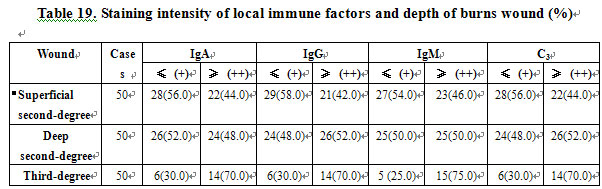
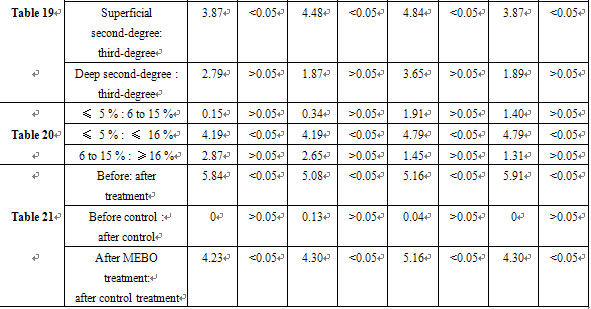
Local immunity was closely related to burn depth. IgA-, IgG-, and IgM-producing cells and C3 in the local area of third-degree burns wounds had stronger staining intensity than those in superficial second-degree burns wounds (P<0.05). The deeper the wound, the stronger the staining intensity (Table 19).
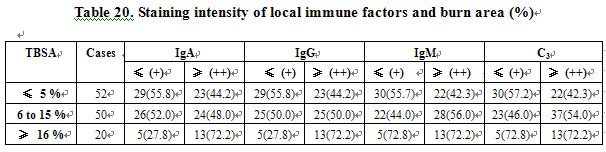
Burn area was positively related to local immune factor staining intensity. IgA-, IgG-, IgM-producing cells and C3 of patients with burn area ≥16 % TBSA had stronger staining intensity than patients with burn area ≤5 % TBSA (P<0.05). The larger the burn area of TBSA, the stronger the staining intensity of the immune factors (Table 20).
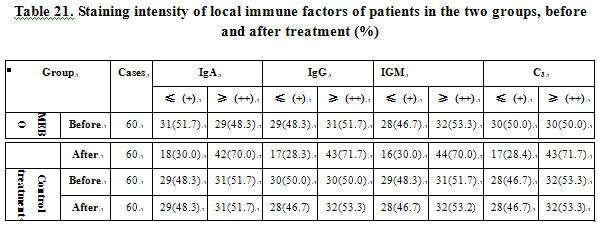
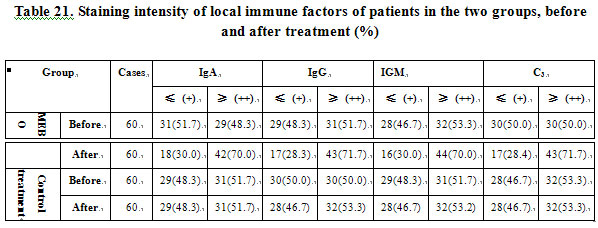
In burns wounds after treatment with MEBO, the local IgA-, IgG-, and IgM-producing cells and C3 had stronger staining intensity than before treatment and than those in the control group (P<0.05). MEBO significantly enhanced the staining intensity of local IgA-, IgG-, and IgM-producing cells and C3, while the Jing Wan Hong ointment treatment group did not shoew a significant effect. (P>0.05, Table21).
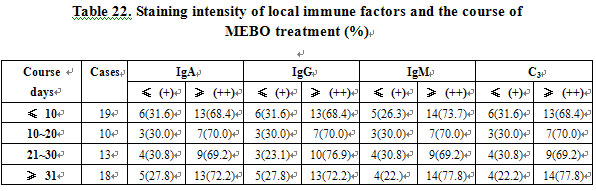
There was no significant correlation between staining intensity of local IgA-, IgG-, ad IgM-producing cells and C3, and the duration of MEBO treatment (P>0.05). The immunity of the patients was enhanced, irrespective of the duration of the treatment (Table 22).
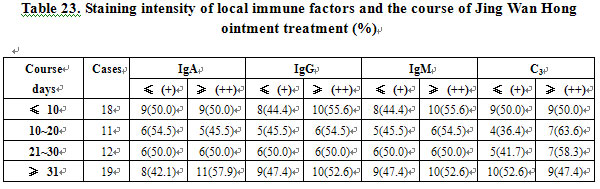
There was no positive correlation between the Jing Wan Hong ointment treatment and the staining intensity of local IgA-, IgG-, and IgM-producing cells and C3 (P>0.05). Changes in staining intensity of immune factors were not attributed to Jing Wan Hong ointment (Table 23).
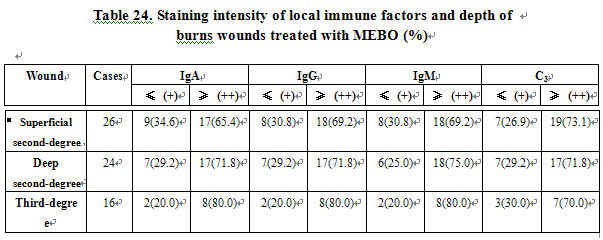
After treatment with MEBO, the deeper the burn wound, the stronger the staining intensity of local IgA-, IgG-, and IgM-producing cells and C3, but no statistical difference (P>0.05). MEBO enhanced the local immunity of different depths of burns wounds (See Table 24).
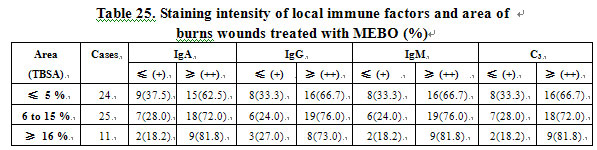
After treatment with MEBO, the larger the burn wound, the stronger the staining intensity of local IgA-, IgG-, and IgM-producing cells and C3, but no statistical difference (P>0.05). MEBO enhanced the local immunity of burn wounds with different area (Table 25).
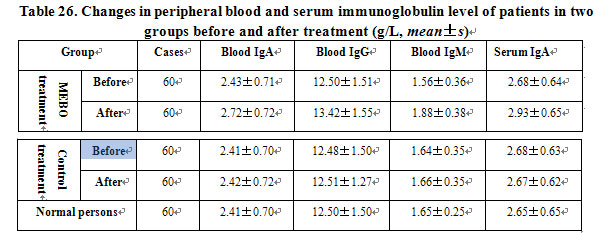
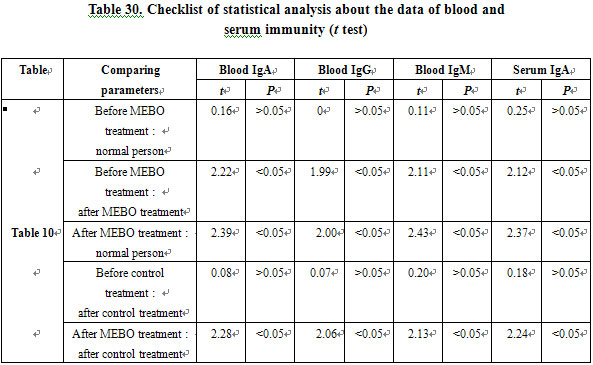
There was no significant difference in peripheral blood IgA, IgG, IgM and serum IgA levels between burns patients and normal persons (P>0.05). After treated with MEBO, peripheral blood IgA, IgG, IgM and serum IgA levels were significantly higher than those of before treatment and those in the control group and normal persons (P<0.05), while in the control group, the before and after treatment difference was not significant (P>0.05). MEBO significantly raised the levels of peripheral blood and serum immunoglobulin (Table 26).
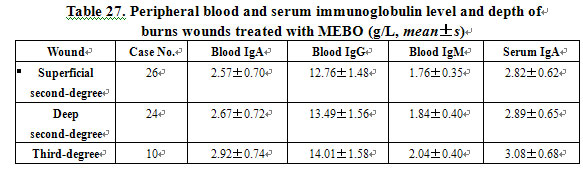
The deeper the burns wounds treated with MEBO, the higher the level of peripheral blood and serum Ig, but no statistical difference (P>0.05). MEBO enhanced the immunity of peripheral blood and serum of patients with different burn depths (Table 27).
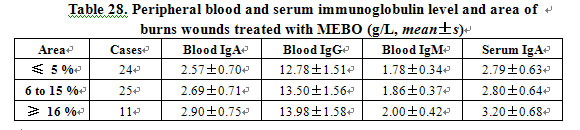
The larger the burns wounds treated with MEBO, the higher the level of peripheral blood and serum Ig, but no statistical difference (P>0.05). MEBO enhanced the immunity of peripheral blood and serum of patients with different burns areas (Table 28). Statistical analysis is shown in tables 29 and 30.
CONCLUSION
The results revealed:
(1) Staining intensity of immune factors at the burn site was significantly higher than that at the non-burn site and in healthy people (P<0.01).
(2) Burns depth and the area had a positive relationship with the local immune factor staining intensity. The deeper and the larger the burns wounds, the higher the staining intensity of the local immune factor and the higher the immunity (P<0.05).
(3) MEBO shortened the healing time of burns wound with different degrees. Compared with the non-MEBO control, the difference was very significant (P<0.01). MEBO promoted healing.
(4) Patients treated with MEBO had their local immune factor staining intensities higher than patients treated with the non-MEBO method (P<0.05).
(5) Patients treated with MEBO had higher peripheral blood and serum immunoglobulin levels higher than before MEBO treatment and also higher levels than patients treated with non-MEBO method (P<0.05). MEBO significantly promoted immunity.
(6) The wound infection rate of the patients treated with MEBO was significantly lower than that of patients treated with the non-MEBO method (P<0.05). MEBO had an antibiotic effect.
The relationship between changes of local and systemic immunity and the depth and the area of burns was also investigated. Through the enhancement of native immunity of burns patients, MEBO was capable of controlling burn wound infection by promoting the endogenous defense to bacteria, virus and toxin invasions as well as through the immune enhancement of burns patients. MEBO shortened the healing time of the wounds.
DISCUSSION
Burns is a severe injury which both destroys the skin barrier and lowers the body’s native defense against bacterial and viral invasions. At the ACCP and SCCM held in August 1991 in the United States, a new definition of infection was advanced [3]: Invasions of exogenous bacteria and virus cause local infection of the burn wound which can progress to systemic infection. Meanwhile, host defenses also induce an inflammatory immunologic reaction. Thus, systemic inflammatory reaction syndrome (SIRS) may result [4]. MEBO itself does not have a direct bacteriocidal effect in vitro. Some researchers considered that MEBO serves as an immunologic barrier in burn wound surface thereby protecting the injured skin. MEBO may create an environment (temperature, humidity, nutrition, oxygen supply, metabolism, etc.) suitable for residual skin tissues repair. In effect, it creates an ideal isolated “aseptic ward”. In addition, MEBO is capable of altering the toxic potential of bacteria and virus in burns wounds therefore lowering the infection rate [5].
This study investigated the effect of MEBO on the local and systemic immunity of burns patients, and proved that MEBO, through regulating human immunity, protected burns wounds from infection at the same time as it promoted wound healing. After MEBO treatment, the incidence of wound infection was reduced to 1.7 %, significantly lower than that in the control group (P<0.05). The average wound healing time in the MEBO treatment group was 23.5±9.3 days, representing a significantly course of treatment as compared with the control group (P<0.01). A vast amount of clinical data proved that MEBO significantly lowered the infection rate of burns wounds when compared with other methods [1]. MEBO is applied directly onto the wound surface and is therefore easily absorbed into the local tissue fluid circulation en route to participation in systemic metabolism. MEBO stimulates the immune system via enhancement of immunoglobulin level and strengthens body resistance against infections. This paper reports the results of local and peripheral blood and serum immunity of patients with different depths and different areas of burns. It proved that MEBO enhanced local and systemic immunologic function as well as enhancing resistance to infection for burns patients.
Determination of local and peripheral blood and serum immunoglobulin level of burns patients is an important criterion for evaluating the effect of MEBO on human immunologic function. IgA, IgG, and IgM are important proteins with anti-bacterial, anti-virus and anti-toxin activities. They also activate complement C3 to achieve bacteriolysis, phagocytosis and neutralization of toxins. C3 takes part in nonspecific and specific immune reactions and is a factor of body defense. It helps to produce immunoglobulin IgA, IgG and IgM. With appropriate regulation of the neurohumoral system, the human body can enjoy enhanced resistance to infectious factors. MEBO contains polysaccharides, lipids and proteins, which in combination and when applied to burns wounds can bind with bacteria and toxins to form protein complexes. These complexes, in turn, stimulate the human immune system, and induce a variation of the bacteria which reduces their toxicity. Therefore, MEBO should not be used together with other topical drugs which may lessen its efficacy. When applying MEBO to the burn wound, the thickness of the ointment should be appropriate since the combination of MEBO with the proteins will be hindered if MEBO is smeared too thickly or too thinly. For the same reason, the time interval of MEBO application should be appropriate.
Before treatment, it was found that the local immunity of the burns patients was higher than in the non-burn area and normal persons. Burns patients with large area and deep wounds had higher local immunity than small area and superficial burns patients. However, the systemic immunity of these burns patients was almost the same as compared with that of normal persons. After MEBO treatment, local and systemic immunity of the burns patients increased significantly more than before treatment and in controls. Therefore, we see that MEBO enhanced local and systemic immunologic function of patients suffering with burns of different depths, different areas and with different courses of treatment. Our results may provide a basis for further research and clinical application of MEBO.
REFERENCES
1. Xu RX: General introduction to medicine of burns, wounds and ulcers. Chin J Burns Wounds Surface Ulcers, 1989, 1: 11-21.
2. Xu RX. The principles of the treatment of burn wounds. Chin J Burns Wounds Surface Ulcers, 1992, 4: 7-21.
3. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ: Definition for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Chest 1992, 101: 1644.
4. Sinclair S, Singer M: Intensive Care. Postgrad Med J 1993, 69: 340-358.
5. Qu YY, Qiu SC, Wang YP, et al: Experimental research on the mechanism of the anti-infection effect of MEBO. Industr Med J 1995, 8: 1-3.