Experimental Study of the Effect of BRT with MEBT/MEBO on He
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
Many researchers found that treatment with BRT with MEBT/MEBO improved the microcirculation in burns wounds. However, the effect of BRT with MEBT/MEBO on systemic postburn situations has not been established. The authors used a rabbit model for the following experimental study on this subject.
MATERIALS AND METHODS
Seventy-two healthy adult rabbits of either sex eating a uniform diet and weighing 2.00.5 kg were divided randomly into three groups, group 1 (normal control, n=12), group 2 (treated with MEBO n=30), and group 3 (dry exposure, n =30). Without anaesthesia, all animals were shaved on the waist with barium sulfide. Animals in group 1 received no treatment and cardiac blood was sampled for measuring normal hematological parameters. Animals in group 2 and group 3 sustained deep second-degree burns of 10 % BSA via 100°C water applied for 5 s (confirmed by pathological examination). Animals in group 2 were then treated with BRT with MEBT/MEBO renewed every 6 h. Animals in group 3 were offered no treatment with wounds remaining dry and exposed. No fluid infusion was administered. Blood samples were taken from left ventricle of heart for determining hematological values at 4, 24, 48, 72 h and 6 days postinjury. The parameters tested included apparent blood viscosity at different shear rates, plasma viscosity, hematocrit (HCT), erythrocyte agglutinative index (EAI) and erythrocyte transformation kinetics (ETK). To standardize the experimental conditions and instruments, blood sampling was performed in accordance with requirements for determination of blood flow viscosity established by the International Council for Standardization in Haematology (ICSH) in 1988. These laboratory determinations were made by a specially assigned technologist at room temperature using a Type NE-1 viscometer (manufactured by Chengdu Instrument Manufactory, China)[1].
Apparent blood viscosity at the shear rates of 230, 115, 46, 23, 11.5, and 5.75 s-1 were determined, respectively, using 1.3 ml blood. Plasma viscosity is the viscosity at the shear rate of 115 s-1. Hematocrit (HCT) was determined by a Wjntrohe tube, type LXJ-64-01 centrifuge, at 3000 rpm for 30 minutes [2]. Erythrocyte agglutinative index (EAI) was the ratio of apparent blood viscosity obtained at low and high shear rates (5.75 and 230 s-1). Erythrocyte transformation kinetics (TK) was calculated according to the formula given in Chen [3].
RESULTS CONCLUSION: Treatment with MEBO after burns could ameliorate total body stress reaction, reduce water evaporation from the wound surface, lessen local and systemic capillary exudation and thus improve the hemorrheological characteristics of microcirculation. It also suggested that when the minor or moderate burned patient was treated with MEBO at an early stage, fluid infusion and/or blood transfusion would not be necessary, whereas for severely burned patients, the amount of fluid infusion could be reduced as tolerated. DISCUSSION Despite becoming a systemic disease, burn injuries begin with a wound on one region of the body surface. It has been reported that BRT with MEBT/MEBO could have both local and systemic therapeutic effects on burn management [6]. We are pleased to report that rabbits in the MEBO-treated group were as active as normal rabbits and fed freely. Blood viscosity did not change significantly (P>0.05), except at shear rates of 11.5s-1 and 5.75s-1 24 h postinjury. The blood viscosity value of normal rabbits in this study was slightly lower than the mean values as indicated in many domestic and international reports. This difference is probably explained by the fact that venous blood from rabbits (weighting 2.5 kg) was sampled in those reports instead of cardiac blood from rabbit (weighting 2.00.5 kg) which we used in our study. Different dietary factors as well as geographical differences may contribute as well. Blood viscosity is a comprehensive marker as in indicates aggregation, deformability and the rheological properties of platelets, RBCs and WBCs. In this study, blood viscosity and plasma viscosity of rabbits were compared to and found to be lower than those of human beings. It remains to be further discussed whether this lower viscosity is associated with low HCT, difficulty of RBC aggregation, or whether it is simply some biological characteristic associated with “herbivores”. REFERENCES
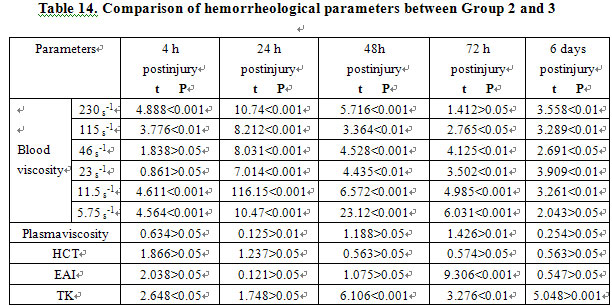
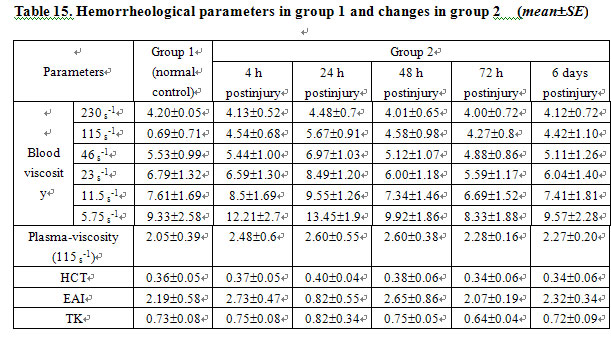
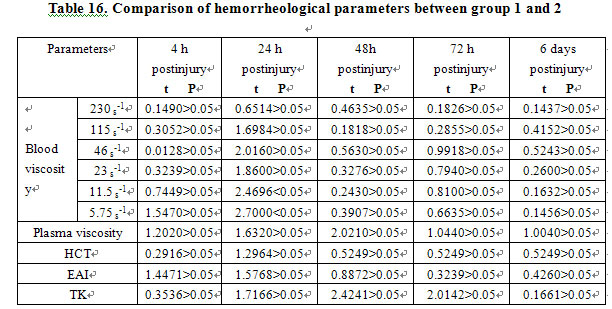
Owing to the minor difference of sex and strain in the hematological parameters of the rabbits, it was feasible to work out a uniform range [1-4]. Randomized division kept animals in a normal control group, allowing the MEBO-treated and the dry-exposed groups to live under the same conditions. Therefore, no repeated blood sampling was allowed and the data were significantly valuable. Apparent blood viscosity and plasma viscosity at different shear rates in group 3 were higher than those in group 2. Table 13 shows that the parameters in group 3 began to increase at 4 h post-injury, peaked at 24 h, and remained higher at 48 h, 72 h and 6 days than those in group 2. There were significant statistical differences (Table 14, P<0.01). Compared to the normal group, parameters including apparent blood viscosity, plasma viscosity and others in the MEBO-treated group began to increase at 4 h postinjury, peaked at 24 h, decreased at 48 h, further decreased at 72 h and nearly returned to normal at 6 days (Table 15). But statistical analysis showed that hematological parameters did not change significantly (P>0.05), except at 24 h postinjury when the blood viscosity at shear rates of 11.5s-1 (t=2.4696, P<0.05) and 5.75s-1 (t=2.700, P<0.05) increased markedly (Table 16).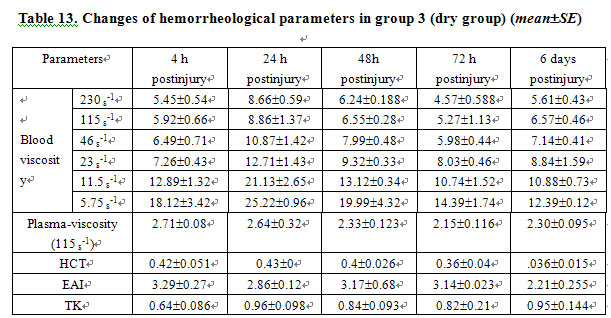
Hemorrhagic change is considered to be one of the pathophysiological changes following burns and serves as a basis of microcirculation disorder. Subsequent to extensive burns, microvascular permeability increases and copious intravascular plasma exudes toward the wound surface and tissue space leading to localized hemoconcentration, reduction of effective blood volume, decreased plasticity of red blood cells and increased blood viscosity. These hemorrhagic changes comprise the pathophysiological basis of burn shock and contribute to the deleterious stress reaction immediately following the trauma of burns. For instance, adrenaline, 5-HT, and prostaglandin may all increase the activation of platelets to erythrocytes, thereby changing the localized electrical potential. The increased secretion of catecholamines due to stress reaction directly promotes platelet adhesiveness. The injured sub-microstructure of the vascular wall elaborates an adhesion protein on platelets and erythrocytes causing significant intravascular platelet aggregation and contributing to adhesion and aggregation of platelets and erythrocyte. This, of course, precipitates thrombotic events [5]. In this study, we compared the blood viscosity of a MEBO-treated group with controls and demonstrate that the viscosity of the MEBO group approximated that of the normal controls. As animals in the MEBO-treated group were treated only with MEBO (they received neither fluid replacement nor special feeding), such changes verified that MEBO alleviated body stress reaction following burns and ensured the body recovery.
1. Du ZY, Jiang XQ: Analysis on hemorrheology of health rabbits. Transact Taishan Med Coll 1991, 12: 134-136.
2. Zhang YM, Jiang XQ, et al: Investigation and analysis on hemorrheological parameters of human health. Chin J Hemato 1992; 13: 312-313.
3. Chen WJ (ed): Hemorrheology. Tianjin: Tianjin Science & Technology Press, 1987; pp 50-53.
4. Guo ZR, et al: Experimental study on the effects of different resuscitation regimens on hemorrheology during burn shock period. Chin J Plastic Surg Burns 1988; 4: 130-132.
5. Xu RX. The medicine of burn and ulcer: a general introduction. Part 1. Chin J Burns Wounds Surface Ulcers, 1989; 1: 11-21.
6. Xu RX. A summary report of the first session of the editorial board of the journal and to the national symposium on the moist exposed burn therapy. Chin J Burns Wounds Surface Ulcers 1992; 4: 2-5.